Poor Sleep Habits Can Rob Years From Your Life
Downloadable White Paper – Sleep/Insomnia PDF
Reestablishing healthy sleep patterns is the most powerful tool you can rely on for health, happiness and longevity. If you’re having difficulty sleeping, consider a drug-free, natural formula to promote healthy sleep to make a real difference.
Sleep is required for human life, enabling critical functions such as those involved in cellular regulation and repair, detoxification, immune health, and hormone level modulation.(1-4) Our physiological homeostasis depends on sleep, yet according to the Centers for Disease Control and Prevention (CDC), one in three adults in the United States does not get enough of it. (5) Given the inextricable linkage between sleep and health, the CDC has warned about the health risks of inadequate sleep, and federal and industry dollars continue to fund research that can help elucidate the roles of sleep in disease and quality of life and to provide solutions for those who struggle with poor sleep.
Developing and maintaining healthy sleep habits may empower people to reduce their risks of illness and disease. Indeed, poor sleep is associated not only with greater risk for developing a host of health problems, including degenerative diseases, Type 2 diabetes, cardiovascular disease, stroke, and attention deficit hyperactivity disorder (ADHD) but also with a greater risk for suffering debilitating symptoms like migraine headaches and for living a shorter lifespan. (9-16)
What is DEEP SLEEP and why is it important?
Deep sleep is also referred to as “slow-wave sleep” (SWS) or delta sleep.
- Your heartbeat and breathing become the slowest they’ll be while you are asleep
- Your brain waves become the slowest they’ll be while you are asleep
- It’s difficult to awaken even with loud noises
Many people never reach deep sleep and sadly miss out on all of the crucial benefits.
What are the benefits of deep sleep?
Deep sleep is where all of the healing, rejuvenating and cellular repair occurs. Reaching deep sleep determines whether you will feel refreshed and alert the next day or groggy and unfocused.
Benefits include:
- energy restoration
- cell regeneration
- increased blood supply to muscles
- growth and repair of tissues and bones
- promotes a strong immune system
Sleep affects all aspect of life
While sleep allows your body to heal and rejuvenate, sleep loss activates undesirable markers of inflammation and cell damage
Sleep…
• Improves your immune function and protects against cell damage
• Supports proper brain function and improves focus, memory, concentration, learning, and productivity
• Lowers your risk of heart disease, diabetes, stroke, dementia, and obesity
• Increases ‘healthspan” (living longer in a healthier state as opposed to living longer in a debilitated, degenerative state
• Affects glucose metabolism and type 2 diabetes risk
• Short sleep duration is one of the strongest risk factors for obesity.
• Poor sleep is linked to depression (sleep affects emotions and social interactions)
One degenerative disease for which there is a growing wealth of research into the role of sleep is the neurodegenerative disease, Alzheimer’s. Alzheimer’s disease is the most prevalent cause of dementia in the older population, accounting for 65 to70% of the cases. The formation of amyloid-β (also known as beta-amyloid or Aβ) plaques and neurofibrillary tangles are the hallmarks of the disease.
People with healthy sleep habits are at a lower risk for developing Alzheimer’s disease and other forms of dementia. (10) Those at lower risk are those who do not suffer from insomnia and who do not experience sleep-disordered breathing (SDB), which includes snoring, sleep apnea, and obstructive sleep apnea. The specific role that sleep plays in protecting against dementia is unclear, but studies have shown that insomnia increases both the production and secretion of amyloid-β, leading to higher levels of amyloid-β in those with insomnia as compared to those with healthy sleep patterns. (17) Research showing that cerebrospinal levels of amyloid-β and its precursor, amyloid precursor protein (APP), are higher at night suggests that it is during sleep that the brain clears itself of these substances. (18) These findings offer some insight into why sleep seems to protect against neurodegenerative diseases like Alzheimer’s.

The sleep-migraine connection: Migraines and other forms of headache can be associated with a variety of diseases and conditions, but they are also known to be associated with lack of sleep. Though the relationship between sleep and migraine is complex,(19) it is clear that the two often co-occur. Indeed, disturbed sleep is more common in adults and children with migraine than those without migraines, with between 30% and 50% of migraine patients experiencing disturbed sleep or poor sleep quality.(20-23) Further, the severity and prevalence of sleep problems increase proportionally with headache frequency, such that the vast majority of chronic migraineurs (68% to 84%) suffer from insomnia on a near-daily basis. (20)
There is evidence that lack of sleep causes migraines and that, conversely, migraines cause loss of sleep. It is therefore likely that migraineurs with disturbed sleep experience a negative feedback loop where migraines and loss of sleep reinforce one another and relief from either condition becomes harder and harder. (20-22) Nonetheless, restful sleep has been shown to be effective in relieving migraine attacks, strongly suggesting that insufficient sleep causes or exacerbates migraine headaches.
Consistent with this view is the finding that those with migraines are less likely to possess the ability to flexibly adapt their sleep/wake cycles (24) and are thus more likely to become sleep deprived. Even more telling is that lack of sleep is the most commonly reported trigger of headaches. (25,26)
NATURAL ALTERNATIVES FOR SLEEP
Alternative headache and migraine therapies include psychological counseling, biofeedback, and physical therapy, which work by making lifestyle changes. Non-pharmacological treatments for the management of migraines and headaches have a growing field of science to support their use. Biofeedback techniques teach patients to control certain responses of their body to help reduce pain. For example, a patient can learn diaphragmatic breathing, heart rate, muscle tension, and how to control the temperature to enter a relaxed state, which may bring about better pain control.
Alternative treatments for insomnia and disordered sleep include background music, acupuncture, prayer, deep breathing, meditation, yoga, and massage.
Non-pharmacological nutritional therapies include natural supplements for sleep which avoids the serious side effects of prescription drugs. Drug-related side effects include kidney damage, ulcers, dependence, addiction, tolerance development requiring higher doses, rebound insomnia, withdrawal symptoms, and daytime grogginess. (19, 20, 21)
Another aspect of over-the-counter NSAID’s (non-steroidal anti-inflammatory drugs) and prescription drugs is that analgesic over-use can cause chronic headache syndrome, where the drug increases the number of migraine episodes per month. Nutritional supplements have never been reported to cause this effect. (22, 23)
FORMULA FOR SLEEP – Nutritional ingredients that have been proven in clinical studies to be of great benefit for people who have difficulty sleeping include:
Hops extract comes from the flowers (seed cones) of the hop plant Humulus lupulus. Hops have long been recognized for its relaxation and calming effect. Studies suggest Hops extract may help to improve sleep quality, shorten time to fall asleep, and improve sleep brain wave patterns.
Valerian extract is a perennial herb native to North America, Asia, and Europe. Studies show valerian may improve sleep quality with fewer night awakenings and greater sleep duration. Valerian is also known for stress reduction and is among the eight most widely used herbal supplements in the world.
Zizyphus Jujube extract is a fruit most frequently used for sleep problems in Traditional Chinese Medicine with little side effects. It is also used for purposes related to gastrointestinal health and digestion and is also known for its relaxation and calming effect.
Glycine is an amino acid that enhances sleep and supports whole-body health. Early research on glycine and its essential role in sleep was published in 1989 and later in 2008. One of the ways in which glycine aids in sleep was clarified when it was discovered that glycine is responsible for the profound muscle relaxation that occurs during various stages of REM sleep. In another study, glycine improved sleep efficiency, reduced difficulty in falling asleep, and enhanced sleep satisfaction.
Vitamin B6 (Pyridoxine HCL) Vitamin B6 (Pyridoxine HCL) helps your body convert food energy into glucose, metabolize fats and proteins, and ensure proper function of your nervous system. With these various effects, there are ways in which your vitamin B-6 status may cause or contribute to your sleeping difficulties, or insomnia. Pyridoxine is considered adequate for neurotransmitter production to support sleep. Studies show that vitamin B6 positively impacts aspects of sleep and is essential for promoting and maintaining a good mood.
Magnesium is involved in over 300 enzyme-related biochemical processes and appears to influence sleep in a variety of ways. Those who are deficient in magnesium are more likely to have abnormal EEG readings during sleep, more nocturnal awakenings, less time spent in stage 5 REM sleep, and self-reports of poor sleep quality. On the other hand, those taking dietary magnesium supplements are more likely to experience better sleep efficiency, the ability to fall asleep faster, and the ability to reduce cortisol levels. Magnesium supplementation also helps to restore normal EEG patterns during sleep.
Melatonin is a hormone produced by the pineal gland that helps to control our body’s biorhythms and thereby helps to regulate sleep. It has become one of the most frequently used non-prescription sleep aids. Melatonin helps to promote total sleep time and can help balance circadian rhythm disruption.
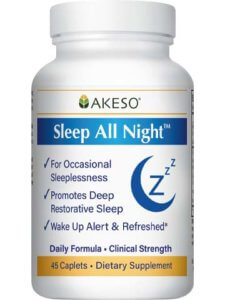
All of these ingredients are included in a new sleep supplement by Akeso Health Sciences called “Sleep All Night.”
Sleep All Night is an effective dietary supplement and powerful sleep aide to promote deep restorative sleep.
Healthy Sleep Benefits Include:
• Allows your body to heal and rejuvenate
• Improves immune function
• Protects against cell damage and reduces inflammation
• Supports proper brain function
• Improves focus, memory, concentration, learning, and productivity
• Lowers risk of heart disease, diabetes, stroke, dementia, and obesity
• Increases “healthspan” (living longer in a healthier state)
• Reduces stress and may reduce depression
INGREDIENTS:
| Vitamin B6 (Pyridozine HCL) | 50 mg |
| Magnesium (Citrate & Oxide) | 250 mg |
| Glycine | 1200 mg |
| Valerian Root Extract (0.8% valerenic acids) | 500 mg |
| Zizyphus Jujube Extract (2% saponins) | 200 mg |
| Hops Extract 4:1 | 100 mg |
| Melatonin | 3 mg |
Read more about the health benefits of deep sleep and Sleep All Night
Related Article – Reset Your Circadian Rhythm
Purchase Sleep All Night
References
- Benington JH, Heller HC. Restoration of brain energy metabolism as the function of sleep. Prog Neurobiol. 1995;45(4):347-360.
- Berger RJ, Phillips NH. Energy conservation and sleep. Behav Brain Res. 1995;69(1-2):65-73.
- Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377. doi:10.1126/science.1241224
- Siegel JM. Sleep viewed as a state of adaptive inactivity. Nat Rev Neurosci. 2009;10(10):747-753. doi:10.1038/nrn2697
- HHS. 1 in 3 adults don’t get enough sleep: A good night’s sleep is critical for good health. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/media/releases/2016/p0215-enough-sleep.html. Published 2016.
- Akerstedt T, Philip P, Capelli A, Kecklund G. Sleep loss and accidents–work hours, life style, and sleep pathology. Prog Brain Res. 2011;190:169-188. doi:10.1016/B978-0-444-53817-8.00011-6
- Wade AG. The societal costs of insomnia. Neuropsychiatr Dis Treat. 2010;7:1-18. doi:10.2147/NDT.S15123
- Leger D, Massuel M-A, Metlaine A. Professional correlates of insomnia. Sleep. 2006;29(2):171-178.
- Malhotra RK. Neurodegenerative disorders and sleep. Sleep Med Clin. 2018;13(1):63-70. doi:10.1016/j.jsmc.2017.09.006
- Shi L, Chen S-J, Ma M-Y, et al. Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep Med Rev. 2018;40:4-16. doi:10.1016/j.smrv.2017.06.010
- Kawakami N, Takatsuka N, Shimizu H. Sleep disturbance and onset of type 2 diabetes. Diabetes Care. 2004;27(1):282-283.
- Bassetti CL. Sleep and stroke. Semin Neurol. 2005;25(1):19-32. doi:10.1055/s-2005-867073
- Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2014;21(1):57-64. doi:10.1177/2047487312460020
- Um YH, Hong S-C, Jeong J-H. Sleep problems as predictors in attention- hyperactivity disorder: causal mechanisms, consequences and treatment. Clin Psychopharmacol Neurosci. 2017;15(1):9-18. doi:10.9758/cpn.2017.15.1.9
- Li Y, Zhang X, Winkelman JW, et al. Association between insomnia symptoms and mortality: a prospective study of U.S. men. Circulation. 2014;129(7):737-746. doi:10.1161/CIRCULATIONAHA.113.004500
- Lin Y-K, Lin G-Y, Lee J-T, et al. Associations between sleep quality and migraine frequency: A cross-sectional case-control study. Medicine (Baltimore). 2016;95(17):e3554. doi:10.1097/MD.0000000000003554
- Wolk R, Gami AS, Garcia-Touchard A, Somers VK. Sleep and cardiovascular disease. Curr Probl Cardiol. 2005;30(12):625-662. doi:10.1016/j.cpcardiol.2005.07.002
- Malhotra A, Loscalzo J. Sleep and cardiovascular disease: an overview. Prog Cardiovasc Dis. 2009;51(4):279-284. doi:10.1016/j.pcad.2008.10.004
- Nagai, M, Hoshide, S, & Kario K. Sleep duration as a risk factor for cardiovascular disease – a review of the recent literature. Curr Cardiol Rev. 2010;6(1):54-61.
- How disrupted sleep may lead to heart disease. nih.gov. https://www.nih.gov/news-events/nih-research-matters/how-disrupted-sleep-may-lead-heart-disease. Published 2019. Accessed April 4, 2019.
- Lao X et al. Sleep quality, sleep duration, and the risk of coronary heart disease: A prospective cohort study with 60,586 adults. J Clin Sleep Med. 2018;14(1):109-117.
- Grandner, MA, Jackson, NJ, Pak, VM, & Gehrman P. Sleep disturbance is associated with cardvascular and metabolic disorders. J Sleep Res. 2012;21(4):427-433.
- Patyar S, Patyar RR. Correlation between Sleep Duration and Risk of Stroke. J Stroke Cerebrovasc Dis. 2015;24(5):905-911. doi:10.1016/j.jstrokecerebrovasdis.2014.12.038
- Koo DL, Nam H, Thomas RJ, Yun C-H. Sleep Disturbances as a Risk Factor for Stroke. J stroke. 2018;20(1):12-32. doi:10.5853/jos.2017.02887
- Sharma S, Culebras A. Sleep apnoea and stroke. Stroke Vasc Neurol. 2016;1(4):185-191. doi:10.1136/svn-2016-000038
- Ma C, Pavlova M, Liu Y, et al. Probable REM sleep behavior disorder and risk of stroke: A prospective study. Neurology. 2017;88(19):1849-1855. doi:10.1212/WNL.0000000000003902
- Phua CS, Jayaram L, Wijeratne T. Relationship between Sleep Duration and Risk Factors for Stroke. Front Neurol. 2017;8:392. doi:10.3389/fneur.2017.00392
- Ooms S, Overeem S, Besse K, Rikkert MO, Verbeek M, Claassen JAHR. Effect of 1 night of total sleep deprivation on cerebrospinal fluid beta-amyloid 42 in healthy middle-aged men: a randomized clinical trial. JAMA Neurol. 2014;71(8):971-977. doi:10.1001/jamaneurol.2014.1173
- Tarasoff-Conway JM, Carare RO, Osorio RS, et al. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015;11(8):457-470. doi:10.1038/nrneurol.2015.119
- Rudnicka AR, Nightingale CM, Donin AS, et al. Sleep Duration and Risk of Type 2 Diabetes. Pediatrics. 2017;140(3). doi:10.1542/peds.2017-0338
- Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529-537. doi:10.2337/dc14-2073
- Tan X, Chapman CD, Cedernaes J, Benedict C. Association between long sleep duration and increased risk of obesity and type 2 diabetes: A review of possible mechanisms. Sleep Med Rev. 2018;40:127-134. doi:10.1016/j.smrv.2017.11.001
- Dutil C, Chaput J-P. Inadequate sleep as a contributor to type 2 diabetes in children and adolescents. Nutr Diabetes. 2017;7(5):e266. doi:10.1038/nutd.2017.19
- Lecube A, Romero O, Sampol G, et al. Sleep biosignature of Type 2 diabetes: a case-control study. Diabet Med. 2017;34(1):79-85. doi:10.1111/dme.13161
- Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Med Rev. 2017;31:91-101. doi:10.1016/j.smrv.2016.02.001
- Zhu B, Hershberger PE, Kapella MC, Fritschi C. The relationship between sleep disturbance and glycaemic control in adults with type 2 diabetes: An integrative review. J Clin Nurs. 2017;26(23-24):4053-4064. doi:10.1111/jocn.13899
- Reutrakul S, Mokhlesi B. Obstructive Sleep Apnea and Diabetes: A State of the Art Review. Chest. 2017;152(5):1070-1086. doi:10.1016/j.chest.2017.05.009
- Walsh JK, Coulouvrat C, Hajak G, et al. Nighttime insomnia symptoms and perceived health in the America Insomnia Survey (AIS). Sleep. 2011;34(8):997-1011. doi:10.5665/SLEEP.1150
- Kelman L, Rains JC. Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache. 2005;45(7):904-910. doi:10.1111/j.1526-4610.2005.05159.x
- Sahota P. Morning headaches in patients with sleep disorders. Sleep Med. 2003;4(5):377.
- Seidel S, Hartl T, Weber M, et al. Quality of sleep, fatigue and daytime sleepiness in migraine – a controlled study. Cephalalgia. 2009;29(6):662-669. doi:10.1111/j.1468-2982.2008.01784.x
- Rasmussen BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain. 1993;53(1):65-72.
- van Oosterhout W, van Someren E, Schoonman GG, et al. Chronotypes and circadian timing in migraine. Cephalalgia. 2018;38(4):617-625. doi:10.1177/0333102417698953
- Spierings EL, Ranke AH, Honkoop PC. Precipitating and aggravating factors of migraine versus tension-type headache. Headache. 2001;41(6):554-558.
- Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27(5):394-402. doi:10.1111/j.1468-2982.2007.01303.x
- Hvolby A. Associations of sleep disturbance with ADHD: implications for treatment. Atten Defic Hyperact Disord. 2015;7(1):1-18. doi:10.1007/s12402-014-0151-0
- Snitselaar MA, Smits MG, van der Heijden KB, Spijker J. Sleep and Circadian Rhythmicity in Adult ADHD and the Effect of Stimulants. J Atten Disord. 2017;21(1):14-26. doi:10.1177/1087054713479663
- Peppers KH, Eisbach S, Atkins S, Poole JM, Derouin A. An Intervention to Promote Sleep and Reduce ADHD Symptoms. J Pediatr Health Care. 2016;30(6):e43-e48. doi:10.1016/j.pedhc.2016.07.008
- Morash-Conway J, Gendron M, Corkum P. The role of sleep quality and quantity in moderating the effectiveness of medication in the treatment of children with ADHD. Atten Defic Hyperact Disord. 2017;9(1):31-38. doi:10.1007/s12402-016-0204-7
- Everitt H, Baldwin DS, Stuart B, et al. Antidepressants for insomnia in adults. Cochrane database Syst Rev. 2018;5:CD010753. doi:10.1002/14651858.CD010753.pub2
- Lu X-M, Zhu J-P, Zhou X-M. The effect of benzodiazepines on insomnia in patients with chronic obstructive pulmonary disease: a meta-analysis of treatment efficacy and safety. Int J Chron Obstruct Pulmon Dis. 2016;11:675-685. doi:10.2147/COPD.S98082
- Asnis GM, Thomas M, Henderson MA. Pharmacotherapy Treatment Options for Insomnia: A Primer for Clinicians. Int J Mol Sci. 2015;17(1). doi:10.3390/ijms17010050
- Lie JD, Tu KN, Shen DD, Wong BM. Pharmacological Treatment of Insomnia. P T. 2015;40(11):759-771.
- Franco L, Sanchez C, Bravo R, Rodriguez A, Barriga C, Juanez JC. The sedative effects of hops (Humulus lupulus), a component of beer, on the activity/rest rhythm. Acta Physiol Hung. 2012;99(2):133-139. doi:10.1556/APhysiol.99.2012.2.6
- Ross SM. Sleep disorders: a single dose administration of valerian/hops fluid extract (dormeasan) is found to be effective in improving sleep. Holist Nurs Pract. 2009;23(4):253-256. doi:10.1097/HNP.0b013e3181aed09d
- Dimpfel W, Suter A. Sleep improving effects of a single dose administration of a valerian/hops fluid extract – a double blind, randomized, placebo-controlled sleep-EEG study in a parallel design using electrohypnograms. Eur J Med Res. 2008;13(5):200-204.
- Koetter U, Schrader E, Kaufeler R, Brattstrom A. A randomized, double blind, placebo-controlled, prospective clinical study to demonstrate clinical efficacy of a fixed valerian hops extract combination (Ze 91019) in patients suffering from non-organic sleep disorder. Phytother Res. 2007;21(9):847-851. doi:10.1002/ptr.2167
- Schellenberg R, Sauer S, Abourashed EA, Koetter U, Brattstrom A. The fixed combination of valerian and hops (Ze91019) acts via a central adenosine mechanism. Planta Med. 2004;70(7):594-597. doi:10.1055/s-2004-827180
- Schmitz M, Jackel M. [Comparative study for assessing quality of life of patients with exogenous sleep disorders (temporary sleep onset and sleep interruption disorders) treated with a hops-valarian preparation and a benzodiazepine drug]. Wien Med Wochenschr. 1998;148(13):291-298.
- Muller-Limmroth W, Ehrenstein W. [Experimental studies of the effects of Seda-Kneipp on the sleep of sleep disturbed subjects; implications for the treatment of different sleep disturbances (author’s transl)]. Med Klin. 1977;72(25):1119-1125.
- Franco L, Sanchez C, Bravo R, et al. The sedative effect of non-alcoholic beer in healthy female nurses. PLoS One. 2012;7(7):e37290. doi:10.1371/journal.pone.0037290
- Dietz BM, Kang Y-H, Liu G, et al. Xanthohumol isolated from Humulus lupulus Inhibits menadione-induced DNA damage through induction of quinone reductase. Chem Res Toxicol. 2005;18(8):1296-1305. doi:10.1021/tx050058x
- Xin G, Wei Z, Ji C, et al. Xanthohumol isolated from Humulus lupulus prevents thrombosis without increased bleeding risk by inhibiting platelet activation and mtDNA release. Free Radic Biol Med. 2017;108:247-257. doi:10.1016/j.freeradbiomed.2017.02.018
- Plazar J, Zegura B, Lah TT, Filipic M. Protective effects of xanthohumol against the genotoxicity of benzo(a)pyrene (BaP), 2-amino-3-methylimidazo[4,5-f]quinoline (IQ) and tert-butyl hydroperoxide (t-BOOH) in HepG2 human hepatoma cells. Mutat Res. 2007;632(1-2):1-8. doi:10.1016/j.mrgentox.2007.03.013
- Oxman AD, Flottorp S, Havelsrud K, et al. A televised, web-based randomised trial of an herbal remedy (valerian) for insomnia. PLoS One. 2007;2(10):e1040. doi:10.1371/journal.pone.0001040
- Pallesen S, Bjorvatn B, Nordhus IH, Skjerve A. [Valerian as a sleeping aid?]. Tidsskr Nor Laegeforen. 2002;122(30):2857-2859.
- Morris CA, Avorn J. Internet marketing of herbal products. JAMA. 2003;290(11):1505-1509. doi:10.1001/jama.290.11.1505
- Ni X, Shergis JL, Guo X, et al. Updated clinical evidence of Chinese herbal medicine for insomnia: a systematic review and meta-analysis of randomized controlled trials. Sleep Med. 2015;16(12):1462-1481. doi:10.1016/j.sleep.2015.08.012
- Rodriguez Villanueva J, Rodriguez Villanueva L. Experimental and clinical pharmacology of ziziphus jujuba mills. Phytother Res. 2017;31(3):347-365. doi:10.1002/ptr.5759
- Shergis JL, Ni X, Sarris J, et al. Ziziphus spinosa seeds for insomnia: A review of chemistry and psychopharmacology. Phytomedicine. 2017;34:38-43. doi:10.1016/j.phymed.2017.07.004
- Hsieh MT, Chen HC, Kao HC, Shibuya T. Suanzaorentang, and anxiolytic Chinese medicine, affects the central adrenergic and serotonergic systems in rats. Proc Natl Sci Counc Repub China B. 1986;10(4):263-268.
- Chen HC, Hsieh MT. Clinical trial of suanzaorentang in the treatment of insomnia. Clin Ther. 1985;7(3):334-337.
- Kwon H, Jung IH, Yi JH, et al. The Seed of Zizyphus jujuba var. spinosa Attenuates Alzheimer’s Disease-Associated Hippocampal Synaptic Deficits through BDNF/TrkB Signaling. Biol Pharm Bull. 2017;40(12):2096-2104. doi:10.1248/bpb.b17-00378
- Chase MH, Soja PJ, Morales FR. Evidence that glycine mediates the postsynaptic potentials that inhibit lumbar motoneurons during the atonia of active sleep. J Neurosci. 1989;9(3):743-751.
- Soja PJ. Glycine-mediated postsynaptic inhibition is responsible for REM sleep atonia. Sleep. 2008;31(11):1483-1486.
- Inagawa K et al. Subjective effects of glycine ingestion before bedtime on sleep quality. Sleep Biol Rythm. 2006;4:75-77.
- Yamadera W et al. Glycine ingestion improves subjective sleep quality in human volunteers, correlating with polysomnographic changes. Sleep Biol Rhythm. 2007;5:126-131.
- Inagawa K et al. Assessment of acute adverse events of glycine ingestion at a high dose in human volunteers. J Urban Living Heal Assoc. 2006;50:27-32.
- File SE, Fluck E, Fernandes C. Beneficial effects of glycine (bioglycin) on memory and attention in young and middle-aged adults. J Clin Psychopharmacol. 1999;19(6):506-512.
- Johansson S, Lindstedt S, Tiselius HG. Metabolic interconversions of different forms of vitamin B6. J Biol Chem. 1974;249(19):6040-6046.
- Russell RM. Factors in aging that effect the bioavailability of nutrients. J Nutr. 2001;131(4 Suppl):1359S-61S. doi:10.1093/jn/131.4.1359S
- Ebben M, Lequerica A, Spielman A. Effects of pyridoxine on dreaming: a preliminary study. Percept Mot Skills. 2002;94(1):135-140. doi:10.2466/pms.2002.94.1.135
- Morris MS, Sakakeeny L, Jacques PF, Picciano MF, Selhub J. Vitamin B-6 intake is inversely related to, and the requirement is affected by, inflammation status. J Nutr. 2010;140(1):103-110. doi:10.3945/jn.109.114397
- Friso S, Jacques PF, Wilson PW, Rosenberg IH, Selhub J. Low circulating vitamin B(6) is associated with elevation of the inflammation marker C-reactive protein independently of plasma homocysteine levels. Circulation. 2001;103(23):2788-2791.
- Sadeghi O, Nasiri M, Maghsoudi Z, Pahlavani N, Rezaie M, Askari G. Effects of pyridoxine supplementation on severity, frequency and duration of migraine attacks in migraine patients with aura: A double-blind randomized clinical trial study in Iran. Iran J Neurol. 2015;14(2):74-80.
- Popoviciu L et al. Clinical and Polysomnographic Researches in Patients with Sleep Disorders Associated with Magnesium Deficiencies. London: John Libbey; 1991.
- Abbasi B, Kimiagar M, Sadeghniiat K, Shirazi MM, Hedayati M, Rashidkhani B. The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. J Res Med Sci. 2012;17(12):1161-1169.
- Nielson, FH, Johnson, LK, Zeng H. Magnesium supplementation improves indicators of low magnesium status and inflammatory stress in adults older than 51 years with poor sleep quality. Magesium Res. 2010;23(4):158-168.
- Tanabe K, Yamamoto A, Suzuki N, et al. Efficacy of oral magnesium administration on decreased exercise tolerance in a state of chronic sleep deprivation. Jpn Circ J. 1998;62(5):341-346.
- Held K, Antonijevic IA, Kunzel H, et al. Oral Mg(2+) supplementation reverses age-related neuroendocrine and sleep EEG changes in humans. Pharmacopsychiatry. 2002;35(4):135-143. doi:10.1055/s-2002-33195
- McGeer PL, McGeer EG. Inflammation and the degenerative diseases of aging. Ann N Y Acad Sci. 2004;1035:104-116. doi:10.1196/annals.1332.007
- Dibaba DT, Xun P, He K. Dietary magnesium intake is inversely associated with serum C-reactive protein levels: meta-analysis and systematic review. Eur J Clin Nutr. 2014;68(4):510-516. doi:10.1038/ejcn.2014.7
- Wagner J, Wagner ML, Hening WA. Beyond benzodiazepines: alternative pharmacologic agents for the treatment of insomnia. Ann Pharmacother. 1998;32(6):680-691. doi:10.1345/aph.17111
- Pandi-Perumal SR, Srinivasan V, Spence DW, Cardinali DP. Role of the melatonin system in the control of sleep: therapeutic implications. CNS Drugs. 2007;21(12):995-1018. doi:10.2165/00023210-200721120-00004
- Pevet P, Challet E. Melatonin: both master clock output and internal time-giver in the circadian clocks network. J Physiol Paris. 2011;105(4-6):170-182. doi:10.1016/j.jphysparis.2011.07.001
- Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Dev Med Child Neurol. 2011;53(9):783-792. doi:10.1111/j.1469-8749.2011.03980.x
- Brzezinski A, Vangel MG, Wurtman RJ, et al. Effects of exogenous melatonin on sleep: a meta-analysis. Sleep Med Rev. 2005;9(1):41-50. doi:10.1016/j.smrv.2004.06.004
- Karasek M. Melatonin, human aging, and age-related diseases. Exp Gerontol. 2004;39(11-12):1723-1729. doi:10.1016/j.exger.2004.04.012
- Ebrahimi-Monfared M, Sharafkhah M, Abdolrazaghnejad A, Mohammadbeigi A, Faraji F. Use of melatonin versus valproic acid in prophylaxis of migraine patients: A double-blind randomized clinical trial. Restor Neurol Neurosci. 2017;35(4):385-393. doi:10.3233/RNN-160704
- Abdelgadir, IS, Gordon, MA, & Akobeng A. Melatonin for the management of sleep problems in children with neurodevelopmental disorders: A systematic review and meta-analysis. Drug Ther (NY). 2018;103(12):1163-1167.
- Janjua I, Goldman RD. Sleep-related melatonin use in healthy children. Can Fam Physician. 2016;62(4):315-317.
- Parker A, Beresford B, Dawson V, et al. Oral melatonin for non-respiratory sleep disturbance in children with neurodisabilities: systematic review and meta-analyses. Dev Med Child Neurol. February 2019. doi:10.1111/dmcn.14157
- Poeggeler B, Reiter RJ, Tan DX, Chen LD, Manchester LC. Melatonin, hydroxyl radical-mediated oxidative damage, and aging: a hypothesis. J Pineal Res. 1993;14(4):151-168.
- Mayo JC, Sainz RM, Tan D-X, et al. Anti-inflammatory actions of melatonin and its metabolites, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK) and N1-acetyl-5-methoxykynuramine (AMK), in macrophages. J Neuroimmunol. 2005;165(1-2):139-149. doi:10.1016/j.jneuroim.2005.05.002
- Carrillo-Vico A, Reiter RJ, Lardone PJ, et al. The modulatory role of melatonin on immune responsiveness. Curr Opin Investig Drugs. 2006;7(5):423-431.
- Bielli A, Scioli MG, Mazzaglia D, Doldo E, Orlandi A. Antioxidants and vascular health. Life Sci. 2015;143:209-216. doi:10.1016/j.lfs.2015.11.012
- Lundmark PO, Pandi-Perumal SR, Srinivasan V, Cardinali DP, Rosenstein RE. Melatonin in the eye: implications for glaucoma. Exp Eye Res. 2007;84(6):1021-1030. doi:10.1016/j.exer.2006.10.018
- Kozirog M, Poliwczak AR, Duchnowicz P, Koter-Michalak M, Sikora J, Broncel M. Melatonin treatment improves blood pressure, lipid profile, and parameters of oxidative stress in patients with metabolic syndrome. J Pineal Res. 2011;50(3):261-266. doi:10.1111/j.1600-079X.2010.00835.x
- Mayo JC, Sainz RM, Antoli I, Herrera F, Martin V, Rodriguez C. Melatonin regulation of antioxidant enzyme gene expression. Cell Mol Life Sci. 2002;59(10):1706-1713.